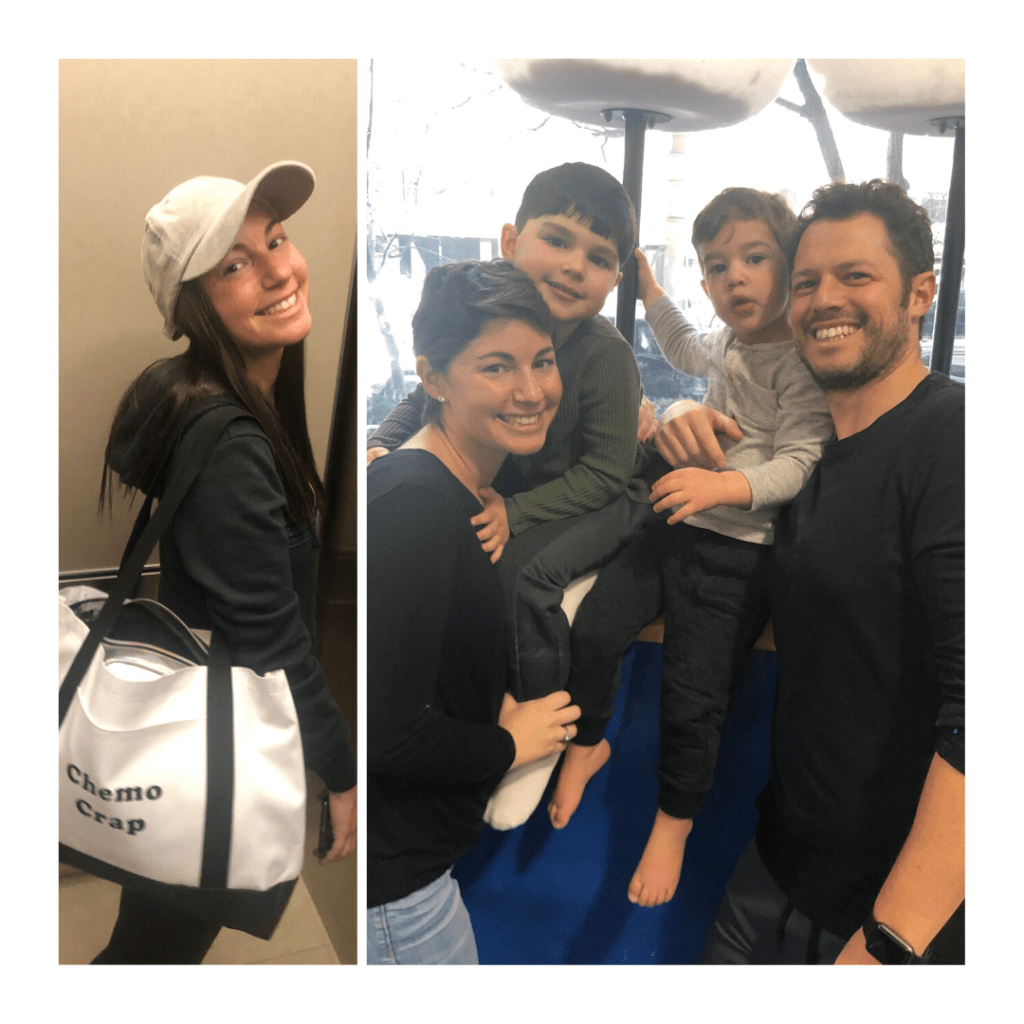
One year ago, on March 25, 2019, I got the call that I have cancer. There aren’t many calls in life that can change your life so dramatically in an instant, but this was one of them. I went from living a normal happy life one day, to being a cancer patient the next.
Throughout all of my treatments and surgeries, I powered forward, never allowing myself to think about unfavorable outcomes. I took it day by day, treatment by treatment, doctor visit by doctor visit. There were days I cried and days I felt great, but overall I just wanted to check 16 chemo treatments off and get through it all.
Well, here we are exactly one year later and I can happily say that I did check those boxes off, had two surgeries, and am now cancer free. When I look back on the last year, I realize how much I have learned about myself in adversity and that even horrible things like getting breast cancer can have silver linings.
During my time going through it all, many friends reached out about different organizations that I should reach out to. One that caught my eye was 5 Under 40, which was dedicated to providing women under 40 (me) with breast cancer (me) or the BRCA gene (me) with medical, beauty, wellness and educational services. Aside from the organization connecting me with a celebrity makeup artist who taught me how to put eyebrows and eyelashes, I loved the group meetups and talking to other women going through very similar things as me.
Most importantly, I’m happy for my health and my family. My older son Aidan said to me the other day, “Mommy, are your boo boos on your boobies all better?” and I was so proud to say yes.
I would be remiss if I didn’t mention my husband Matt who has been an incredible rock during all of this, handling everything with amazing balance and knowing what I needed and when I needed it. On our wedding day in his vows, he said that he would be my rock, and like a rock, I might want to throw him sometimes. Well, he was right on with both, but I couldn’t be luckier to have him as my rock. I love you.
I am so grateful for the rest of my family, friends, friends of friends that all reached out and helped me through the last year. I can’t even express how much it all meant and I am beyond thankful to have such amazing people in my life.
1 year down, forever to go. #Shaystrong